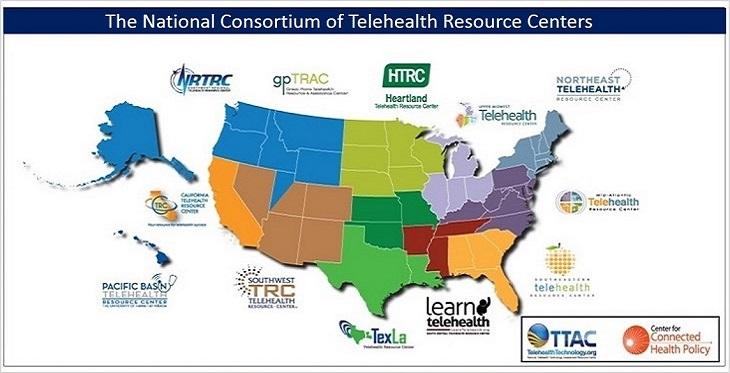
The Telehealth Resource Centers (TRCs) have been in existence for just over 10 years, with the SWTRC for nearly all of that time. In honor of this decade of service to the telehealth community the TRCs released a 10-year report summarizing our group and individual accomplishments and services (available upon request). Periodically it helps to sit back and reflect a bit on what we’ve accomplished as we chart our course for the next few years.
Southwest Telehealth Resource Center Blog

In the beginning…
Using the strictest definition, telemedicine has been around since the ’60s. Initially it was medical professionals with a phone and a video screen consulting with one another. Since the users in question were both regulated and overseen by state boards of medicine, this use often didn’t require many additional rules or regulations.
The patient-provider relationship is a sacred bond that has existed since the dawn of healthcare. The trust and responsibility placed on the provider by the patient to heal and act with their best interest in mind remains at the core of this relationship even in the modern age of healthcare.
The Southwest Telehealth Resource Center (SWTRC) and its parent organization, the Arizona Telemedicine Program (ATP), launched their Service Provider Directory at their first Telehealth and Telemedicine Service Provider Showcase, in Phoenix in October 2014.

Rural healthcare is suffering, but many communities have yet to swallow the medicine that could make a difference: telemedicine.
Several vectors have led to what the National Rural Health Association estimates is more than 50 rural hospital closures over the past five years, with 12 already closing in 2016 so far. The challenges that rural healthcare face include a high percentage of uninsured and elderly patients, reduced populations, equipment that is not fully utilized, and the lack of lucrative specialty services that help support hospitals financially. There also are the issues of getting patients to rural hospitals in a timely manner due to travel distances, and luring top talent from larger cities.
Telemedicine can address many of these issues if rural communities take the opportunity seriously.