Children have long been recognized as a population with significant challenges accessing medical care, most notably due to a limited number of pediatric specialists who are concentrated at children’s hospitals in urban settings. And the very nature of face-to-face, traditional health care may place a disproportionate burden on low-income and rural based families.
This is particularly true in the large geographic region served by Children’s Hospital Colorado and the University of Colorado School of Medicine.
For several years we have partnered with primary care practices, other hospitals, and public health departments to offer outpatient tele-specialty care in underserved communities, and educational and practice support partnerships. But we are rapidly moving toward our goal of an integrated telehealth model that uses a range of technology tools to bridge geographic and communication gaps across the spectrum of pediatric health care.
This has required an innovative, multidisciplinary approach to growth.
Pediatric telehealth programs are most effective when they provide care integrated into local patient-centered medical homes, instead of adapting existing adult telehealth models to children. With this approach in mind, telehealth services that we support span the continuum of care and vary according to the needs of each community. For example:
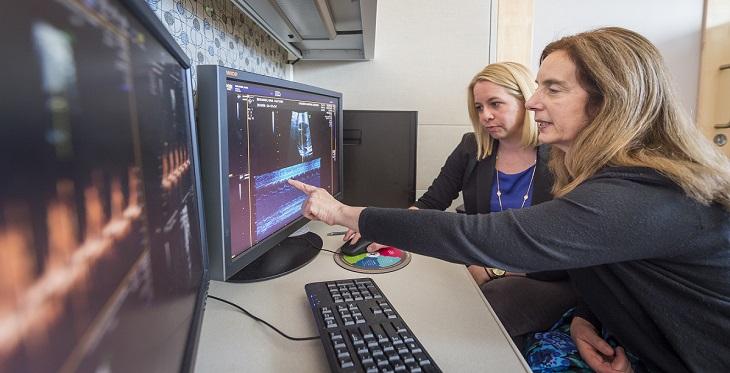
- Fetal cardiology to augment in-person services at a maternal-fetal medicine practice
- Multi-specialty appointments at primary care pediatric practices
- Orthopedics, neurology and rehabilitation appointments at county public health departments for children with neuromuscular diagnoses
- Child protection team consults, and foster care family “coaching”
- Care transition handoffs to primary care providers when complex neonatal ICU patients are discharged from Children’s Colorado back into their home communities
- Training school nurses how to administer intranasal midazolam during seizures
- Training and tele-mentoring for school nurses managing chronic health conditions through Project ECHO (Extension for Community Healthcare Outcomes) communities of practice
- Project ECHO tele-mentoring modules to build PCPs’ base knowledge on complex pediatric diagnoses, such as psychoactive medication management
- One-hour “PEAKS” sessions to augment community practitioners’ existing knowledge base with clinical pearls and the latest research-based recommendations on topics such as diabetic ketoacidosis management
- Home-based neuropsychology visits for children recovering from concussions
- Psychiatric safety evaluations by clinical social workers in emergency rooms and urgent care centers
When adult-focused telehealth programs expand into pediatrics, it is important to note that pediatric financial models are heavily driven by Medicaid policies. By and large, Medicaid telehealth policies in the southwest region go beyond CMS’s telehealth guidance for Medicare although there are exceptions. With the advent of national health reform and Medicaid expansion, state Medicaid programs have a particular interest in telehealth as they work to provide high-quality care at less cost. However, variability among state Medicaid programs mean that pediatric telehealth programs serving a multi-state region must know the policies in each state. It is also worth noting that commercial payers often use Medicare guidance as a reference point for their telehealth policies, including those for pediatric beneficiaries.
Telehealth for children is also unique in that technology must adapt to children of different sizes with varying developmental abilities, and camera lens angles need to be wide enough to capture at least two people – the patient and a parent – in a room.
Patient verification, consent and confidentiality procedures should also conform to state laws regarding minors. However, once these additional items are addressed, children and parents of young children tend to be very comfortable with technology because they have grown up with technology in many other areas of their lives.
Children may even be more comfortable with telehealth than trips to the doctor’s office or a hospital, since they are accustomed to building and maintaining virtual relationships through social media and gaming environments. The pediatric telehealth operating procedures developed by the American Telemedicine Association and endorsed by the American Academy of Pediatrics provide excellent process and technology recommendations for telehealth programs that care for children, although they do not provide clinical guidance.
Telehealth-specific clinical guidance for children is minimal, although most professional society clinical care guidelines for in-person pediatric care are equally applicable to telehealth.
Telehealth can improve access to critically important health care not only via virtual consults, but also by increasing individual provider and health care system capacities across large geographic regions. Our telehealth program is pioneering innovative projects while conducting patient outcome and cost research. These projects are designed to integrate pediatric telehealth into health systems throughout the region. to achieve the quadruple aim – improved health, a better experience of care for patients and families, lower costs, and improved provider satisfaction.


